Coagulation Heart Attack and Stroke – Part 2
It is necessary to understand the interaction of fibrin coagulation pathways and platelet aggregation. Once we understand these interactions we can then discuss current treatment modalities. My goal is to show you a more creative and natural approach to anti-coagulation.
Initial Platelet Aggregation
In part one I emphasized the importance of platelet aggregation as the initial step. There is an initial injury to an arterial or venous wall. As a response, activated platelets cause a clumping reaction to repair the injury. Somewhat like Hans Brinker’s “finger in the dike.”
This injury could be a laceration. It could be a rupture of a atheromatous plaque. It could simply be a tear in an arterial wall. Or simply from low-flow stasis. Atrial fibrillation is an example.
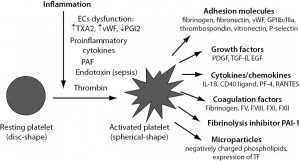
You can see from fig 2 above that the platelets initiate an array of reactions. I will elaborate even more detail in the next post. This is ever-increasing overview.
Aspirin is the most common drug to prevent platelet aggregation. We will look at an array of drugs that have been used over the years. But there is a more creative approach.
Once the initial platelet plug has formed the long-term fibrin coagulation pathway is initiated.
Fibrinogen pathways
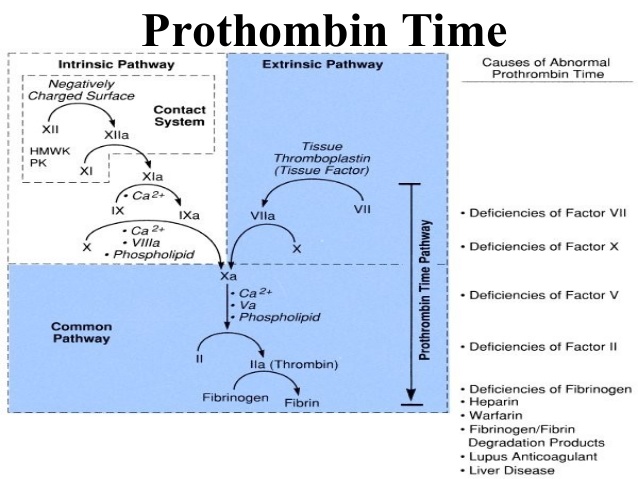
The classic fibrin clotting pathway is divided into the intrinsic and extrinsic systems. The intrinsic system starts with Factor XII. There is a cascading series of reactions to the final common pathway. This is prothrombin activating thrombin. Thrombin then catalyzes the reaction of fibrinogen to fibrin. Finally, fibrin is polymerized to an insoluble mesh. The extrinsic arm interacts with the intrinsic arm.
As discussed previously, the production of fibrin can be blocked at various stages. The conversion of fibrinogen to fibrin can be reversed through a process called fibrinolysis. An important concept.
So now we have a complete picture. The following diagram summarizes the evolution of this thrombus from platelet aggregation to fibrin clot.
Decision-making – Blocking Which Pathway?
Now we have rapidly covered the two aspects of thrombosis (clot) production. This is where the subject becomes indeterminate. Some “guidelines” emphasize the prevention of platelet aggregation. While other guidelines emphasize the long-term use of anti-fibrin drugs. What is the best strategy? Depends on the guidelines. These evolving guidelines are determined by age, associated risk factors, and preceding condition.
These guidelines were originally developed to make decision-making simple. And uniform. And coherent. The community standard of care. But guidelines eventually become bloated and incoherent. Much like IRS tax code. I anticipate this decision-making process will soon be totally computerized. Remove the human discretionary input. I do not agree. Look here to see just how complex this decision tree for anticoagulant therapies can be.
The entire purpose of this series of posts is to present a novel combination of anti-fibrin anti-platelet modalities.
Now you have an overview of the basic flow. In part 3 we will examine current and past drug interventions.