AntiPlatelet AntiCoagulant Drugs
Coagulation and Anticoagulatant Therapy
Read part I and part II of this series for background. So you will have a basic understanding of coagulation pathways. Yes, it is complex.
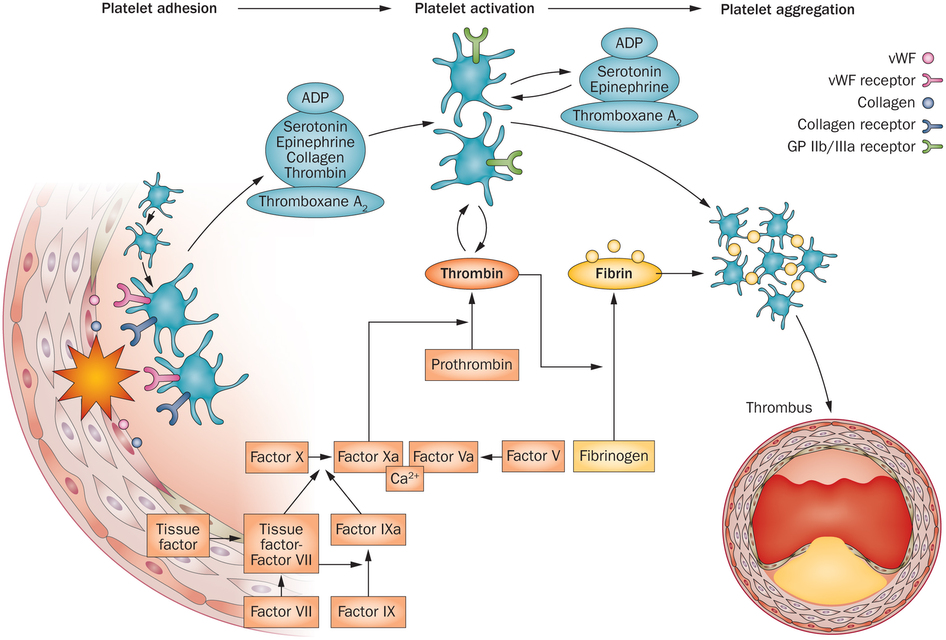
Remember, coagulation or clotting starts with platelet aggregation. That initiates the complex coagulation cascade. This causes the mature thrombus or blood clot. Aggregated platelets with a thick fibrin mesh causes the thrombus. The thrombus causes heart attacks, strokes or thrombophlebitis. Here is the final complete picture:
So let’s discuss anticoagulant therapy medications.
Antiplatelet Agents – Aspirin and Plavix are first line of defense
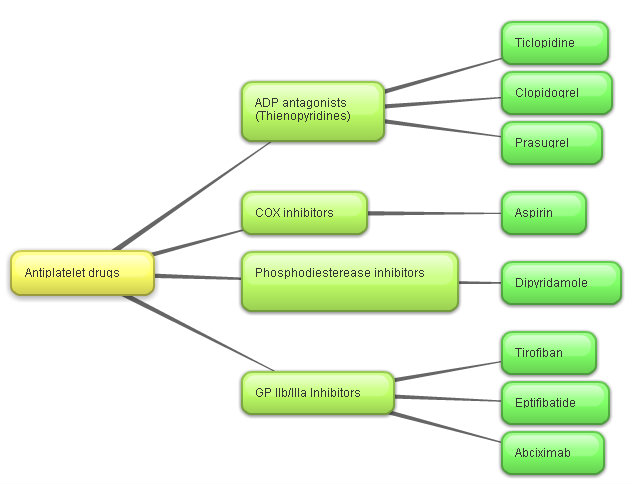
Figure 2 shows how we prevent platelet aggregation and activation at various stages. Look at figure 1. Aspirin has been the mainstay of antiplatelet therapy. There has been a succession of drugs over the last three decades. Newer antiplatelet drugs supersede older ones. Are these true advances or simply marketing campaigns?
Aspirin has been well studied in the literature. A full 325 mg dose will prevent platelet aggregation. Over time, aspirin has significant adverse reactions. These are direct and indirect reactions. It can cause tinnitus (ringing or buzzing noises in the ear). It can cause major gastrointestinal bleeding. This is a significant problem.
Therefore, baby aspirin (81 mg) is a reputedly safer dose. This lower dose is effective. We now know this is subject to individual variations. Fast or slow metabolizers. There are ways of testing for aspirin efficacy. Aspirin Resistance (11-Dehydrothromboxane B2) is one available test. Realistically, we rarely perform this test. So that empirically, an 81 mg (baby aspirin) dose is less toxic. Interestingly, we rarely treat babies and toddlers with baby aspirin any longer.
Aspirin is a COX inhibitor. COX is an acronym for cyclo-oxygenase. There are COX-1 and COX-2 enzymes.
Fish oils are potent COX inhibitors. I will talk about Fish Oils in the final chapter – part 4.
Plavix (Clopidogrel) is now the second most commonly prescribed drug in the US. A 75 mg dose is common. Plavix is an ADP antagonist. A totally different site of action from aspirin. Plavix combined with aspirin has never been a rational choice. It is over treating, potentially causing more complications. Various studies have proven this. Lancet argument against using Plavix and aspirin together:
Adding aspirin to clopidogrel in high-risk patients with recent ischaemic stroke or transient ischaemic attack is associated with a non-significant difference in reducing major vascular events. However, the risk of life-threatening or major bleeding is increased by the addition of aspirin.
Dr Mercola also writes:
Sadly, Plavix also has serious side effects you may not be aware of. Six years ago, I warned my readers that when combined with aspirin, the drug nearly doubled the death rate from heart disease among patients who had not had a previous heart attack but were at risk, compared to those taking aspirin alone.
Anti Fibrin and Standard Anticoagulant Drugs – Coumadin
During acute episodes in hospital, physicians use heparin. This is intravenous dosing. Once discharged, physicians prescribe Coumadin (Warfarin) for long-term therapy. Yes, Warfarin is rat poison.
Typically, Coumadin anticoagulant therapy is continued for a variable period of time depending on the condition. Coumadin blocks vitamin K -dependent conversion steps. So you are advised not to ingest any extra vitamin K. Or foods that are high in vitamin K such as leafy green vegetables.
Prothrombin time (PT) was used in the past to monitor the efficacy and dosing of Coumadin which is quite variable. Today we use the INR (international normalized ratio). Weekly monitoring is necessary initially. Then less frequently as the INR activity stabilizes. But I stress, there is considerable variability in dosing from 2 mg up to 12 mg.
A typical Coumadin dose is 5-6 mg daily.
Coumadin has serious adverse consequences because it blocks vitamin K. Matrix GLA is a vitamin K-dependent protein that regulates calcium flow. It prevents prevents “reverse calcium flow.” That is, calcium flowing out of the bones into the arteries (and heart valves). Coumadin can accelerate osteoporosis and arterial calcification. That is why high doses of vitamin K in healthy adults is so vital. So the risk-benefit ratio seems questionable. Here is one journal citation
Fourteen years ago in this journal, Price and colleagues reported that 2 weeks of warfarin treatment in young rats “caused massive focal calcification of the artery media” (1). It had been known for years that Warfarin could induce mineral deposition in the arteries of rodents (2), and the phenomenon was so robust that Warfarin was often used as an experimental model for vascular calcification, but the mechanism was unknown.
Newer Anticoagulant – Xa (10a) blockers
So time marches on. Newer drugs, with which are not vitamin K antagonists, are now the “latest advance.” These are Xa (10a) antagonists. They eliminate the variability of Coumadin dosing and the necessity for frequent testing. And we suspect marketing decisions are in play.
What are these newer drugs?
- Dabigatran Etexilate – Pradaxa 150 mg twice daily
- Rivaroxaban – Xarelto 20 mg daily
- Apixaban – Eliquis 5 mg twice daily
- Edoxaban – Savaysa 60 mg daily
These newer drugs avoid frequent monitoring. What are the downsides? There are no currently available “antidotes” to unintentional overdose. Vitamin K is a simple antidote to Coumadin. And, long term, there are consequences yet to be fully determined. In one study from BMC Musculo-skeletal Disorders, there was a direct toxic effect on osteoblasts. These are the cells that build new bone:
In conclusion, rivaroxaban and enoxaparin treatment led to a reduction in alkaline phosphatase activity and a reduction in BMP-2, osteocalcin and Runx2 mRNA expression, indicating that treatment with both drugs leads to a general negative effect on osteoblast activity.
The Medical Letter lists these as the major toxic effects. Common to all anticoagulants:
The most common adverse effect of edoxaban in clinical trials was bleeding. Edoxaban has no established antidote to reverse its anticoagulant effect, which persists for about 24 hours after the last dose, and it is not dialyzable. Epidural or spinal hematomas resulting in permanent paralysis could occur in patients taking the drug who require neuraxial anesthesia or spinal puncture.
We will eventually discover other long term consequences. This class is certainly far more convenient. And way more expensive.
So let us turn our attention in the final Part 4 to a comprehensive and time-tested natural anticoagulant routine.
2 thoughts on “AntiPlatelet AntiCoagulant Drugs”
Thank you for writing. Vitamin K2 MK7 and 45 µg is a very tiny dose. Keep reading the blogs with a much more robust discussion of the differences between MK4 and MK7. Vitamin K2 does not “thicken the blood” or “cause clots.” There should not be a significant interaction between aspirin and vitamin K2.
Are there any contradictions taking 45 mcg of vit k2 mk7 while on low dose of aspirin 75 mg .?
Or May be vit k2 Will be a safe guard of bleeding from the use of aspirin.
Appreciate your comments for there contradicting information
Of using both aspirin together with vit k2