Estrogen and Migraine Headaches
Does estrogen benefit or exacerbate migraine headaches? Common knowledge in the medical literature is that estrogen may increase the frequency and severity of migraine headaches. This has not been our experience.
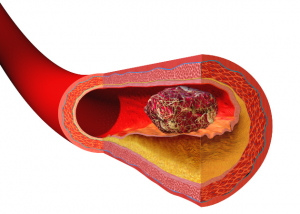
Estrogen is a vasodilator. And, therefore, should prevent the constricted phase of migraine headaches.
So let me tell you a clinical story. A 52-year-old postmenopausal female patient went to see her gynecologist. On pelvic ultrasound her endometrial (uterine lining) thickness was 4 mm. At her age a “normal” endometrial thickness is <4 mm. Anything greater > 4 mm is considered “thickened” and therefore some cause for concern. It is assumed that her age there is no hormonal stimulation of the endometrium. This requires an expanded discussion.
She was advised to stop her estradiol estrogen therapy. So she weaned herself off her estrogen over 1 to 2 weeks. But then began experiencing an increased frequency of migraine headaches. So much so that she began taking the anti-migraine medication, Imitrex, every day. Now the upper recommended frequency of Imitrex is no greater than 9 tablets monthly. That is because Imitrex is a vasoconstrictive that can cause significant systemic vascular ischemia — lack of oxygen delivery.
And sure enough she began to experience a rapid heart rate with some chest pain. She went to her local emergency room where she was diagnosed as a sudden and new case of atrial fibrillation. She was given some intravenous Diltiazem which should have slowed and reconverted her heart rhythm. This was unsuccessful after two doses. So the attending staff decided she should be cardioverted. This requires sedation and an electrical shock to the chest to convert the heart to a normal rhythm. She was then referred to a cardiologist for further workup.
Needless to say, a dreadful and “shocking” series of events. OK. Pun intended.
I have postulated over the last 25 years that the final common pathway of estrogen is choline production. Choline is vagotonic. That will slow the heart and increases normal and healthy secretions. During menopause estrogen levels decline and so do choline levels. The body reactively increases dopamine levels. This is what we call a sympathetic discharge. This is experienced as hot flashes, night sweats, nervousness, anxiety, cognitive difficulties, itching and in this case cardiac arrhythmias. All of these have been reported in postmenopausal women in their fifties.
We reinstituted her estradiol (Minivelle) patch, changing every 3 days to maintain consistent levels. And in this situation prescribed very low dose Inderal – a beta blocker.
The headaches have ceased. An unfortunate situation where estrogen withdrawal was ill advised leading to a series of rather distressing and significant consequences.
Lessons to be learned. Estradiol estrogen has over 400 vital functions.
Philip Lee Miller, MD
Carmel, CA
Aug 2019