Is Cholesterol the Culprit?
Probably as long as you can remember, cholesterol is “known” to be the cause of cardiovascular (heart and blood vessel) disease. Does dietary cholesterol cause heart disease? What about familial super high cholesterol? Does that cause heart disease? The short answer is – probably not. Let’s expand. I have written extensively on the subject in the past.
Cholesterol has been studied since the early 1900s. Initially in fits and starts. John Goffman studied cholesterol in the 1950s at Donner labs in Berkeley. There was no interest. So he turned to other pursuits. The cumulative effects of low level radiation. Lipid research picked up in the 1970′ and 80’s.
Remember, the admonition to limit your egg consumption consumption? Or fats? You should reduce fats to reduce your weight. We have now found it didn’t work. My good friend Dr. Ron Rothenberg famously quips, “cholesterol: found at the scene of the crime – not guilty.” How do we prove this assertion?
cholesterol: found at the scene of the crime – not guilty. — Dr. Ron Rothenberg
Rudolph Virchow in the 19th century postulated that most human disease is a result of inflammation. Most especially cancer, but probably vascular disease as well. Later Sir Thomas Sydenham postulated, “a man is as old as his arteries.” So we have historical precedents for the cause of cardiovascular disease– inflammation.
“a man is as old as his arteries.” — Sir Thomas Syndenham
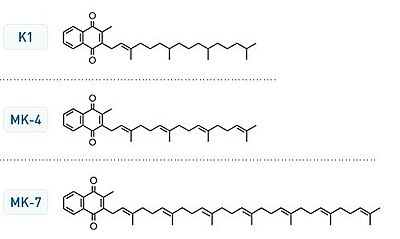
When I was young medical student, we looked at total cholesterol. Over time the entire picture has evolved with more and more refinements and “precision.” So we now look at LDL, HDL, and VLDL. These are actually lipoprotein carriers of cholesterol and not cholesterol itself. LDL cholesterol is transported to the heart initially for repair. HDL is the reverse cholesterol transport system carrying cholesterol away from the heart. This has come under more intensive scrutiny in the last few years.
Further refinements have followed, including Lp(a), LpPLA2, myeloperoxidase, hs-crp, homocysteine, uric acid, and now particle counts. Let me return to this in a minute.
The goal of conventional cardiologists is reducing LDL numbers to less than 100 mg/dl or for “at risk” patients – as low as 60-80 mg/dl. Does this make any difference?
Dr. Daniel Steinberg was one of the most notable researchers in lipidology while I was at UCSD School of Medicine. He wrote The Cholesterol Wars. A good read for its historical content. At one point, he notes, “we almost lost the battle until statins arrived.” Which implied that severe dietary restriction alone was insufficient to reduce cardiovascular morbidity and mortality. Statins were much more potent. We could lower LDL more aggressively. But is reduction of LDL successful? I contend not. Statins are anti-inflammatory. They do not work by simply lowering LDL levels as much as mitigating inflammation.
That is why statins may actually have the greatest effect and benefit surrounding the acute period of a myocardial infarction.
Berkeley Heart Lab (BHL) pioneered the concept of LDL particle sizing. This has drawn more recent attention and acclaim. BHL developed the notion of pattern typing using an expensive and laborious gel electrophoresis process. Which, in its day, superseded the expensive and neglected ultracentrifuges used by John Goffman. He had access to the warehoused ultracentrifuges that were originally designed to refine uranium during the super secret Manhattan Project at Berkeley Lawrence Lab and Sandia Labs.
Pattern A is characterized by low triglycerides, high HDL and large, fluffy LDL particles which are presumably less atherogenic. That is, they cause less vascular disease. A pattern B is characterized by high triglycerides, low HDL and small dense atherogenic LDL particles.
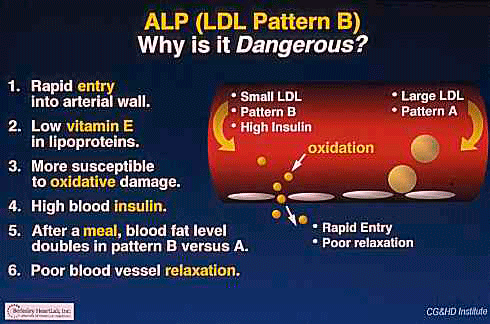
So we think particle sizing and LDL size may be a good marker of future pathology or disease. Again, large and fluffy LDL particles are less dangerous. Small dense LDL particles are far more pathogenic and atherogenic. This may be an impaired paradigm.
Dr. Robert Superko, co-founder of BHL, has been lecturing and advocating since the early 1990s on the danger and pathogenicity of Pattern B. He was aggressively trying to raise HDL and thereby lower heart disease with high dose Niacin. Empirically, we do see patients who have high HDL’s are at less risk. Unfortunately, therapeutic trials to increase HDL with niacin or experimental drugs (torcetrapib) have not been successful. I have often asked why is that? That may be the subject of a future blog. Milano A1 and HDL2b.
It is very likely we are missing or misinterpreting this picture. The real risk is high triglycerides which are carbohydrate induced, increasing the risk of diabetes and glycation. A series of events leads to increasing hemoglobin A1c levels (glycation), arterial stiffening, hypertension, and increased cardiovascular disease.
The most unfortunate, but glaring example was Tim Russert. He was known to have normal cholesterol but very high triglycerides. He died at the age of 58. Quite premature. What is the lesson here? Pattern B may be a biomarker for glycation because of its increase in triglycerides which are associated with higher carbohydrate intake. We see this as increased hemoglobin A1c levels.
Glycation is the end result of AGE products – Advanced Glycation End-Products. Which, by the way, was one of the postulates of my book the Life Extension Revolution: Growing Older without Aging.
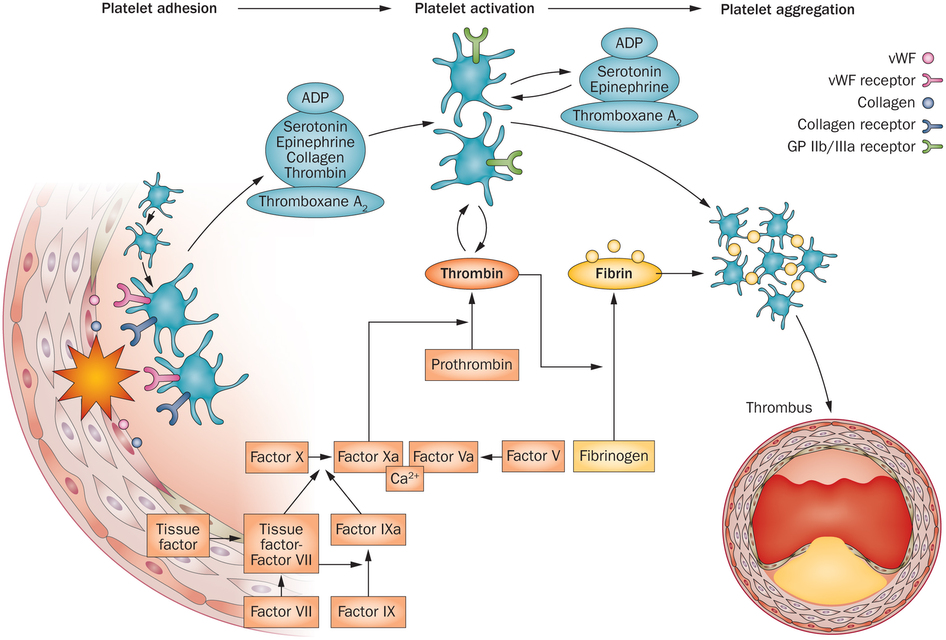
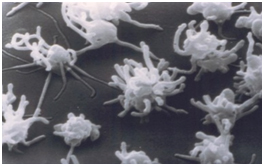
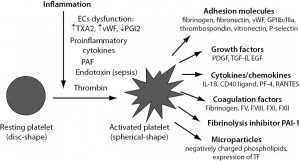
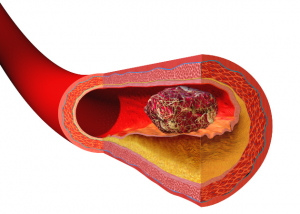
Now let’s add another seriously overlooked cause of cardiovascular disease. Adhesion molecules. VCAM-1 is the most notable. Vascular Cell Adhesion Molecule. These adhesion molecules are highly active in cancer and in cardiovascular disease. It initiates a cascade of inflammatory responses where white cells and macrophages are drawn (recruited) into an inflammatory process forming arterial plaque. The end result of this inflammatory process is aggregated white blood cells and macrophages. That is soft plaque. This is, in essence, a pustular aggregation within the arterial wall. Somewhat like acne on the face, but rather in the intimal-medial aspect of your arteries.
Most unfortunately, Medicare and most insurance companies who follow suit, do not reimburse or recognize advanced cardiovascular risk factors. Most of the medical community does not see cardiovascular disease as an inflammatory process. We are stuck in an old paradigm that overindulgence of fat and cholesterol causes heart disease. There is no incentive economically or even medically to go beyond simple LDL measurements. Guideline derived, algorithmic medicine is short-circuiting our progress.
“without deviation from the norm, progress is not possible” – Frank Zappa
The real test of pathogenicity is imaging studies. Carotid intimal medial thickness (CMIT) measures arterial wall thickness and developing plaque. Superfast (EBT) CT scans (HeartScan) scores calcium load in your coronary (heart) arteries. Even a simple blood pressure measurement gives you valuable clues about arterial compliance and glycation. This is directly visualizing actual disease.
LDL and cholesterol is a bad predictor of eventual cardiovascular disease and events.
Empirically, I have seen this most vividly in specific cases. Extremely high familial LDL levels with entirely normal vascular studies. And extremely low LDLs associated with repeated coronary artery blockages requiring stents.
Now, I want you to read my detailed review of the major cholesterol studies that I published here in June 2015. This shows the results of all the major statin induced cholesterol lowering studies using absolute statistics and not relatives statistics. There was virtually no survival advantage on a population basis from statins. On an individual basis, there may be lives saved. But on a population wide basis there was no change. Totally contrary to what you have heard. What physicians believe or “know.” But it is based on rigorous statistical analysis using absolute and not relative statistics.
Bottom line: We need to change the paradigm.
We should be using new and more appropriate biomarkers for risk determination based on an inflammatory profile.
Triglycerides may be more pathogenic than cholesterol.
Low carbohydrate intake. Carbs are killing us. Don’t overeat.
Moderate exercise.
Stress reduction.
Update and revise our entire therapeutic protocols.
Look at diabetic risk using HgA1c as a glycation biomarker.
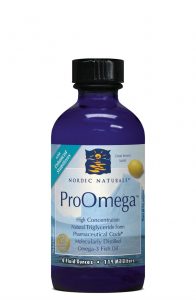
High dose fish oils.
Appropriate anti-oxidants.
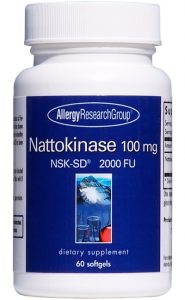
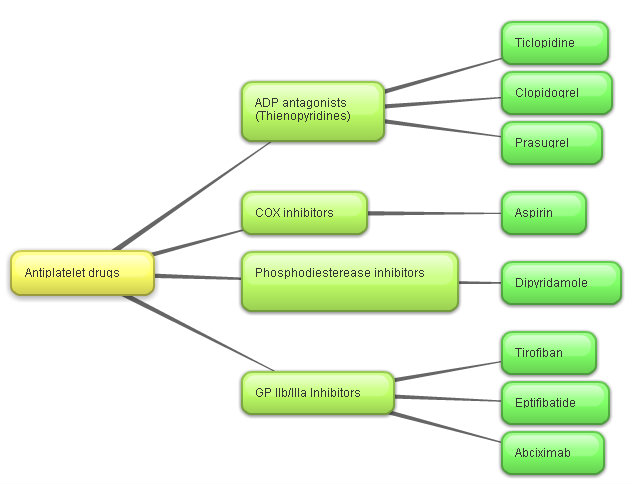
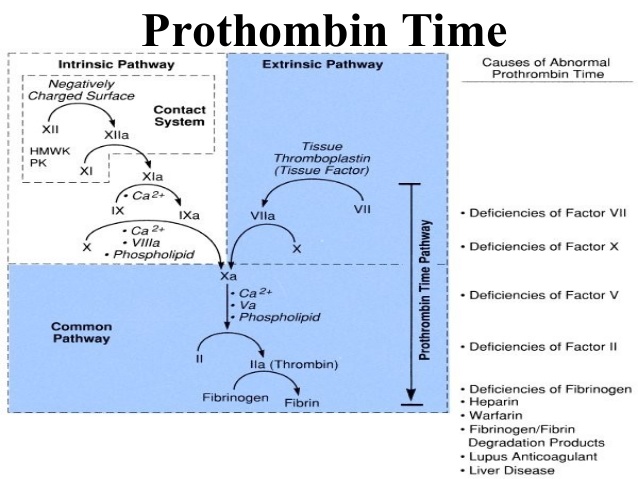
Prevent heart attacks and strokes with my natural anti-coagulant routine.
Let me know what you think.
Philip Lee Miller, MD
Carmel , CA
December 7, 2018