Statins: A Critical Appraisal
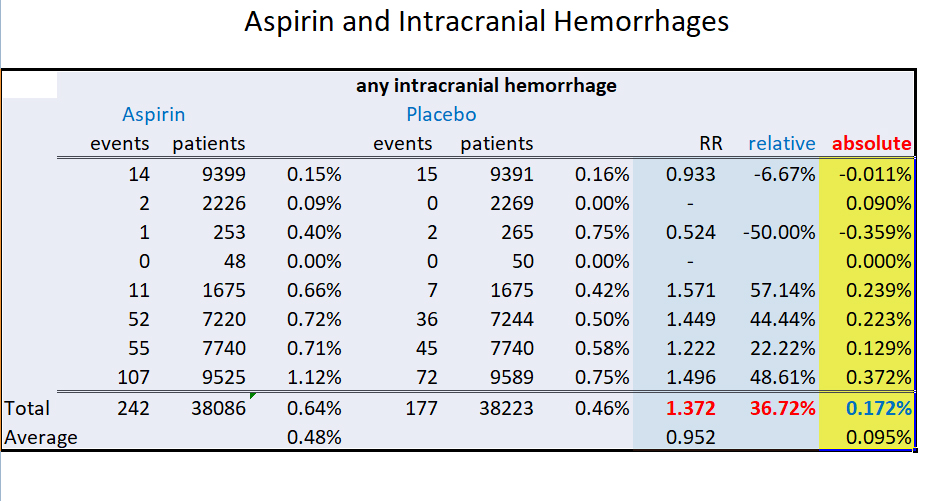
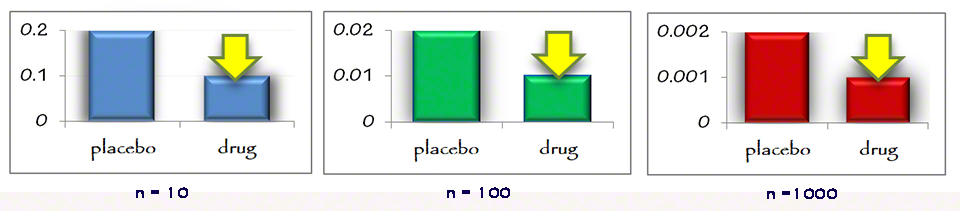
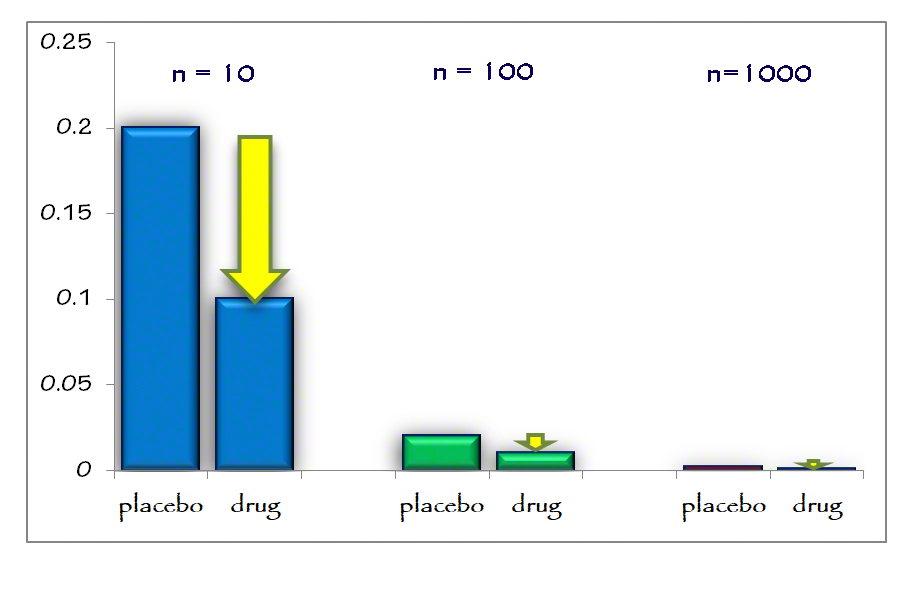
You can find a number of well written books with articulate statistical analyses over the years questioning the results of statin therapy. What is the true value and efficacy of statins (HMG-CoA reductase inhibitors) in treating and preventing heart disease? The statistics can be overwhelming. What is the real risk benefit ratio?
Lipids and the Emergence of Statin Therapy
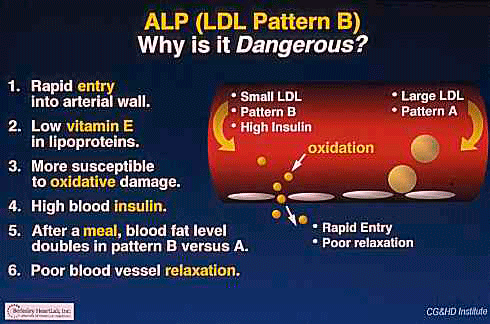
Lipid research actually started sometime in the early 1920’s. It gained more momentum in the 1950’s with John Gofman at the Laurence Radiation Lab in Berkeley. Then the interest waned, so the field languished for another few decades. John Gofman turned his energies to examining and warning us of the dangers of constant low level radiation therapy
In the 1950’s and 1960’s the cholesterol theory was gaining more adherents. Anyone over 50-60 remembers well the exhortation to eat less fat. No eggs. Skimmed milk. Substitute margarine for butter. It was much healthier. Cholesterol was bad. Turns out margarine is literally the bottom of the barrel stuff. Highly hydrogenated oils. Much less healthy. Personally, I never believed the cholesterol theory even in Medical School and was labeled a heretic. “Dummy, everyone believes the cholesterol story.”
One of the most erudite and gentlemanly Professors at UCSD Medical School was Dr. Daniel Steinberg, a prominent lipid researcher. He wrote a wonderful book The Cholesterol Wars which is one of the best historical accounts of the lipid research over the past 80 years. He even admits “we almost lost the cholesterol debate if it had not been for the emergence of Statins.”
The Framingham Study was a large study begun about 45 years ago in a small town outside of Boston where a majority of the population has been studied annually. It is the best cross sectional study we have.
Interestingly, even the Framingham study proved that cholesterol is a bad predictor of heart disease. 50% of those who suffered heart attacks had totally “normal” cholesterol levels. By the way, the term “normal” is a moving target and subject to standards committee declarations. There is no “normal” cholesterol, only declared “acceptable levels.” A GP, an internist or a cardiologist will have different and increasingly aggressive definitions of “normal.”
Association vs causality is an ancient debate which is not well settled. Aristotle proposed four postulates for causality. Many centuries later, David Hume, the great Scottish Enlightenment philosopher expounded about this in detail.
Cholesterol does not cause heart disease. …