Vitamin K, Calcification and GLA Proteins
Vitamin K2 is a potent anti-calcification nutrient via GLA protein carboxylation. Let’s look at this process of calcification and the potency of these various forms of vitamin K2. Then talk about the MK-4 vs Mk-7. Which is best for you? And why?
Vitamin K2 forms
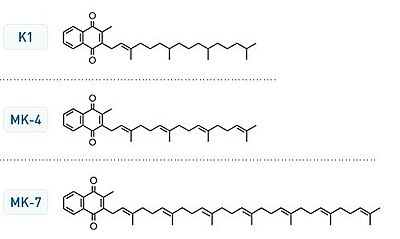
There are currently three forms of vitamin K available. Vitamin K1 (phylloquinone) has been extensively studied. It is not the most potent form. Vitamin K2 is currently available in two forms. MK-4 also known as menaquinone-4 or menatetranone. MK-7 (menaquinone-7) is currently advocated as the most potent form of vitamin K2. You can see in fig 1 that the MK-4 and MK-7 have long “tails” with multiple (poly unsaturated) double bonds. This increases lipid solubility. These are fat soluble as opposed to water vitamins.
So what is the connection between Vitamin K2 and tissue calcification? Why do we petrify as we grow older? Why do we grow stiffer? This is a combination of calcification and glycation. Glycation is secondary to excess carbohydrates, rising hemoglobin A1c (>5.6%), and impaired fasting blood sugars (>100 mg).
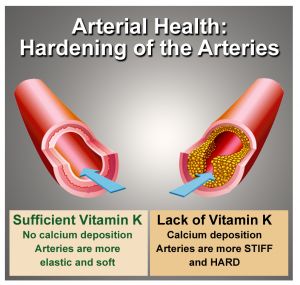
Calcification is an impaired healing process. Arterial injuries initiate a process of calcium deposition as a repair mechanism. Calcification is the end result of chronic inflammatory processes. This is a key concept.
How can we prevent or reverse this ossification process?
For many years I have struggled to understand the process of “reverse calcification.” As we grow older there is a tendency to lose bone calcium matrix causing osteopenia or osteoporosis. And contrariwise, an increase in arterial and cardiac (heart) valvular calcification. When we were younger, calcium deposition was a bone building process. As we age it becomes a cardiovascular risk.
Coumadin as an Experimental Model
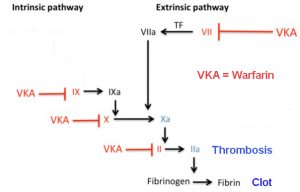
As it turns out, we have an excellent model from widespread use of Coumadin (Wafarin) anticoagulation. From empirical observation over 20 years and through extensive medical literature research, it is now proven that Coumadin accelerates osteoporosis and arterial calcification – coronary artery disease. How is that possible? Because Coumadin’s main action is antagonizing vitamin K2 action. That is the goal. Depleted Vitamin K thins the blood. It inhibits thrombosis and emboli (blood clots). Fig 2 shows the essential vitamin K-dependent steps that are blocked. [refer back my earlier discussion of coagulation and the prevention of heart attacks and strokes]
Now the good news is high doses of vitamin K2 does not cause the opposite. It does not cause abnormal clotting or thickening. The Japanese have carried out experiments using high doses of vitamin K2 for up to two years without any untoward effects. Even the World Health Organization has not determined an upper limit of vitamin K intake. It is only the insufficiency or blockage of vitamin K2 that thins the blood.
Carboxylation of GLA Proteins
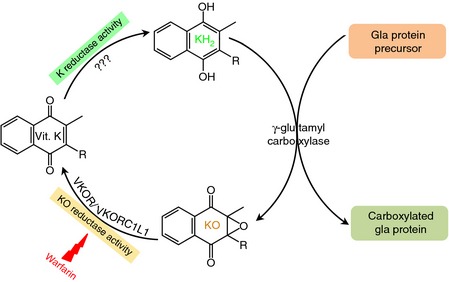
Now the rest of the vitamin K2 calcium connection is the effect on GLA proteins. These are proteins that are absolutely essential for calcium regulation. And this is where so much of the vitamin K research has been focused. The activation of these GLA proteins are all Vitamin K dependent. See figure 3 the Vitamin K cycle. Once again, notice where warfarin blocks the final production of the active form of vitamin K (KH2) that is essential for carboxylation.
So what are these GLA proteins? This is a contraction or acronym for gamma-carboxyglumatic acid proteins. Each one of these is essential for calcium regulation. The most important of these include:
- Osteocalcin (BGP — bone GLA proteins)
- MGP (matrix GLA proteins)
- GRP (GLA rich proteins)
- and more
Experimentally, these proteins have been classified as either under-carboxylated (ucMGP or ucOC) or sufficiently carboxylated (cMGP or cOC). Under-carboxylated forms of these GLA proteins promotes vascular and valvular calcification. There is a rare syndrome – the Keutel Syndrome — characterized by abnormal calcifications and defective MGP. Now refer to figure 4.
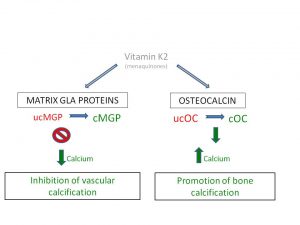
The picture is now complete. You want healthy inflow of calcium for strong bones. We want to reverse or prevent calcium outflow and accumulation in arteries and heart valves. Vitamin K2 as MK-4 or MK-7 are potent activators of matrix GLA proteins (MGP) and Osteocalcin.
We have long struggled with this paradox. Progressive arterial calcification leading to coronary artery disease or peripheral vascular disease. Very little attention has been focused on valvular calcification which is even more serious. Eventually leading to open heart surgery with aortic or mitral valve replacements.
My friends in the alternative community at ACAM (American Academy for Advancement in Medicine) have long advocated the use of chelation therapy. Chelation therapy uses EDTA and other micronutrients infused intravenously to reverse calcification. Various alternatives to intravenous EDTA include oral and even rectal suppositories with some degree of success.
To further strengthen this connection let’s consider one final pathologic model. Chronic renal disease. Refer to figure 4.
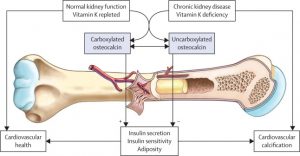
Repeating, Osteocalcin is essential for bone building and health. It is a strong biomarker for vitamin K levels and activity. Osteocalcin must be carboxylated to exhibit full activity. Under carboxylated Osteocalcin is not fully active. It is totally Vitamin K2 dependent. So measuring ucOsteocalcin (under carboxylated) is a stronger biomarker for Vitamin K2 activity. Until recently this test was not available. This is slowly changing. Genova Diagnostics is one source.
MK-4 vs MK-7 Research
A large body of research on the phylloquinone or vitamin K1 form has been conducted. It has been concluded that this is an insufficient approach to the carboxylation of the GLA proteins. So that more recent experimentation with MK-4 has demonstrated sufficient potency to activate the carboxylated GLA proteins.
Then the MK-7 form was investigated. MK-7 is naturally found in the natto bean which is the source of Nattokinase. So much of the controversy currently is focused on MK-4 versus MK-7. Both of these are lipids soluble as previously mentioned..
Extensive literature research will reveal various shortcomings. Most experiments fail to use good basic pharmacological principles of the dose response curves. That is, what is response at various doses.
I frequently use the example of Lipitor. If we conduct an experiment with 1 mg of Lipitor for 1 to 5 years as an example, we will conclude that Lipitor is ineffective at lowering LDL. On the other hand, if we use a dose of 100 mg Lipitor for even one year we will find a very high rate of significant side effects intolerances and eventual discontinuation of the drug. So based on the initial dose we will find an appropriate response.
I have often questioned how researchers even pick the initial dose of any agent they are studying. What is this decision-making process?
So there have never been direct comparisons between high doses of MK-4 and MK-7. The Japanese of studied vitamin K2 (MK-4) in doses up to 30 to 40 mg (30,00 – 45,000 µg). These are “attack” doses. MK-7 has been tested in doses initially from 45 µg and much more recently as high as 400 µg. But there are no studies that compare head-to-head high doses of MK-4 with high dose of MK-7.
So Which Form of Vitamin K2 is Best for Me?
All we know is that researchers have concluded that even the “high” doses of MK-7 do not fully carboxylate the GLA proteins. So what is the appropriate dose of MK-7? Some researchers speculate it may be as high as 1000 µg.
I contend that both are lipid soluble. There are various factors including lipid solubility, volume of distribution (Vd), half-lives and ultimately carboxylation of GLA proteins. That is the goal. It is not serum levels. It is not half-lives. It is what is the optimal dose that fully carboxylates these GLA proteins? Especially MGP – matrix GLA protein and osteocalcin. There is a realization that this is the realistic approach.
So you will read that MK-7 is more potent than MK-4. This is primarily based on persistent blood levels of the MK-7 version. There is a difference between lipid solubility, tissue activity and blood levels. Even I measure serum levels of all hormones knowing that there are other part compartments such as saliva, urine.
Now I am beginning to see a combination of MK-4 and MK-7 to “hedge your bets.” We do not know the ideal dose. We do know that there is no upper dose of vitamin K that is toxic. This is why am now recommending at least 30 mg (30,000 µg) of vitamin K2 in the MK-4 version in at-risk patients. While 15 mg is my standard daily dose of Vitamin K2 MK-4. The MK-7 dosing is still in evolution. There is a sense that 400 µg is far more potent than the 45-90 µg that you have currently been taking in various combinations.
Conclusion
The reverse calcification paradox is solved. The experimental evidence is so compelling. Vitamin K2 is essential for healthy arteries and heart valves. This extends to healthy veins as well. The only controversy or decision is the form?
MK-4, MK-7 or a combination of both? Some of this will be practically solved by prices. What is more “affordable” to you? In the end it is all so much more efficient and less expensive than even a single day in a hospital or an extended ER visit.
I continue to recommend 15-30 mg of the MK-4 but remain open to a combination. I always had difficulty rationally understanding how 45 mcg of MK-7 was more potent than 15,000 – 30,000 mcg of MK-4. That would be at least 666 times. Nearly 3 orders of magnitude? I have seen no evidence in the literature to prove this assertion.
The real issue is monitoring. We have been testing Vitamin K with SpectraCell analysis for the last 20 years. Testing functional sufficiency levels. ucMGP and ucOS, as they are more available, will be the real test of Vitamin K efficacy. Will we see evidence of calcification reversal and increased bone density with higher doses? Imaging studies can confirm effectiveness of our therapies. Carotid ultrasound, CIMT (carotid intimal media thickness), ultrafast CT HeartScans and DEXA scans.
Take your vitamin D3 and Vitamin K2 together. My unfailing recommendation to you for the last 15-20 years.
PostScript
I want to personally thank Lara Pizzorno for help with background literature research. Her writings on Vitamin K are highly recommended.
References and Bibliography
[1] Rogier Caluwe, Lotte Pyfferoen, Koen Boeck, An S. De Vriese: Effects of vitamin K supplementation vitamin K antagonists on progression of vascular calcification: ongoing randomized controlled trials. Clinical Kidney Journal, 2016, volume 9, no 2, 273-279
[2] Elke Theuwisse, Egbert Smit, and Cees Vermeer: The role of vitamin K in soft tissue calcification. Adv. Nut 3: 166-173, 2012
[3] Masataka Shiraki andNaoko Tsugawa, Toshio Okano: Recent advances in vitamin K -dependent GLA containing proteins and vitamin K nutrition. Korean Society of Osteoporosis 2015
[4] Takafumi Okura, Mie Kurata, Daijiro Enomoto, Masanori Jotoku, Tomoaki Nagao, Veena Raiska Desilva, Jun Irita, Len Ichi Miyoshi, Jitsuo Higaki: Under carboxylation of osteocalcin is a biomarker of carotid calcification in patients with essential hypertension. Kidney Blood Pressure Res 2010, 33:66-71.
[5] Rick H van Gorp and Leon J. Schurgers: New insights into the pros and cons of the clinical use of vitamin K antagonists (VKA’s) versus direct oral anticoagulants (DOACs). Nutrients 2015, 7, 9538-9557; DOI: 10.3390/nu7115479. citation link
[6] Toshiro Sato, Leon J. Schurgers and Kazuhiro Uenishi: Comparison of menaquinone-4 and menaquinone-7 bioavailability in healthy women. Sato et al nutrition Journal 2012, 11. citation link
[7] Ellen G.H.M.van den Heuvel, Natasha M. van Schoor, Paul Lips, Elke J.P. Magdeleyns, Dorly J.H. Deeg, Cees Vermeer, Martin den Heijer: Circulating un carboxylated matrix GLA protein, a marker of vitamin K status, is a risk factor of cardiovascular disease. Maturitas 77 (2014) 137-140 1 citation link
Philip Lee Miller, MD
California Age Management Institute
Monday, October 10, 2016
8 thoughts on “Vitamin K, Calcification and GLA Proteins”
The main difference is the longer tail MK7 enhances AUC (area under the curve) sustained blood levels. There is no predeliction of bone vs arterial based on this configuration. What the detailed text demonstrates is persistence or blood levels does not guarantee increased effectiveness. Enhanced tissue and cellular concentrations is the goal. And the doses currently in vogue are insufficient to fully carboxylate Matrix GLA proteins. Thank you for your question
I thought that MK4 is beneficial for bone health and MK7 is for reducing arterial calcification? Do I have that correct?
Thanks in advance!
Hello Dr. Miller. I have had tension headaches for 20 years straight. I am very calcium sensitive. I know for a fact it makes it worse. I have better trying to to figure what would bring relief. Magnesium has been most helpful to date, and now I am finding vitamin k2 is helping too. I think its because of both their relation to calcium. I have had very stiff neck, violently twitching muscles in my scalp, heart palpitations, inability to swallow, just a lot of things having to do with constricted muscles. Do you see any feasibility in K2 being helpful in my situation. Are there any tests you’d recommend?
There’s no wrong with vitamin k2, no matter what chain it is (mk-4,mk-7,mk-9 etc.) The longer the chain is the longer is the half life in your blood stream and also the absorbtion increases. The reason why some people experience different reactions may be dose wise or supplemental form.
Thank you for your comments. There is no evidence that Vitamin K2 has an anti-coagulant effect — thins the blood. That is why every user of standard anti-coagulants is cautioned to never eat foods with or supplement with vitamin K2. Nobody knows anything is a rather broad statement. You might want to read this series in its entirety once again.
Half of the internet says vitamin K thins the blood (NOT deficiency of Vit K), and the other half says vitamin K thickens the blood.
Nobody knows anything.
Vitamin K2 as a supplement gives me sudden bruises, for no reason. Green vegetables in my diet do not cause any odd bruising.
I’ll stick to eating the vegetables.
Excellent questions Gary. Most of the research in the literature surveyed did not mention magnesium contribution. Yes, magnesium is highly beneficial. And incidentally, high levels of phosphate are also very harmful.
The best test is ucMGP not ucOC. Advice from Dr. Cees Vermeer, the leading reseacher in the world. Low magnesium can be assessed directly with RBC magnesium or SpectraCell functional testing.
What is the role of magnesium in tissue calcification? Low magnesium is associated with higher calcification. Could the GLAs be fully carboxylated yet calcification still occurs if magnesium is low? Would the blood test for ucOsteocalcin also be a marker for low magnesium in addition to low K2?
Nicely researched and written article!